Retinal Conditions
Diabetic Retinopathy & Macular Degeneration
Diabetic Retinopathy
Diabetes can affect the blood vessels in the retina, causing them to become either blocked or leaky, which can cause loss of vision in some cases.
The risk of this damage increases with:
- Increased duration of diabetes
- Higher average blood sugar levels (poor diabetic control)
- High blood pressure and cholesterol
- Smoking
People with diabetes should have their eyes checked regularly by an eye care professional with experience in this area, as early detection and appropriate treatment can prevent vision loss. They should also minimise their risk by having regular visits with their General Practitioner, to monitor and minimise the above risk factors.
Macular Degeneration
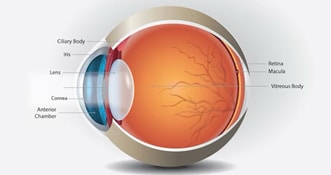
The macula is the central area of the retina, the thin layer of tissue at the back of the eye with the light sensitive cells essential for our vision. The macula is the specialised area in the central retina that is responsible for our detailed, fine central vision for tasks including reading.
Macular degeneration is a group of conditions that cause damage to this area, resulting in loss of detailed vision, but in which peripheral or side vision generally remains preserved. It is a leading cause of blindness in Australia.
The main risk factor for Macular Degeneration is age. Other risk factors include family history of Macular Degeneration, smoking, high blood pressure and cholesterol.
There are two main types of macular degeneration – wet and dry. In Dry MD, the retina and underlying tissues gradually show signs of wear and tear, resulting in vision deterioration that is usually slowly progressive. There is no currently available treatment, but research is continuing.
In Wet MD, abnormal blood vessels form under the retina that can leak fluid and bleed, which distorts vision and damages the light sensitive cells of the macular region. Untreated, Wet MD often results in a rapid deterioration in central vision. Unlike Dry MD, however, treatment is often possible. Usually this involves a series of injections to stop the leakage from the abnormal vessels.
Ophthalmologists are well trained in detecting and treating macular degeneration, giving the best chance of preserving vision.
FLASHES AND FLOATERS
(VITREOUS DEGENERATION)
Symptoms of floaters (small dark shadows that appear to float in your vision) and flashes of light with no apparent source can result from degeneration of the vitreous (the clear jelly filling the back 4/5 of the eye). The vitreous is clear and quite solid when we are young, but begins to break down as we get older, forming liquid pockets within it. Sometimes as it breaks down, small clumps of connective tissue can cast shadows on the retina (the thin film inside the back wall of the eye responsible for vision – a bit like the film in a camera) causing floaters.
Often, the vitreous degenerates to the point that it ‘collapses’ on itself. When this happens, the thicker outer part of the vitreous can peel away from the retina (known as a ‘vitreous detachment’). In most cases, this causes no problems (other than the nuisance value of the floaters). In a small number of patients, the vitreous may tear a small hole in the retina as it peels away. When this occurs, fluid can seep through the hole and under the retina, resulting in a ‘retinal detachment’ (see below), which can cause loss of vision.
Prompt detection and treatment of a retinal tear can prevent progression to a retinal detachment. Treatment usually involves application of laser around the tear, to prevent fluid from spreading under the retina. Therefore, anyone with the following symptoms should have their eyes examined promptly by an eye care professional:
- New onset of flashing lights, especially if accompanied by new floaters
- A sudden increase in the number of floaters seen in your vision
- A dark shadow or curtain in your peripheral, or side vision. This can be a sign of a detachment developing, and is an urgent problem, as it can cause permanent reduction if the detachment spreads to the central vision, even if subsequent surgical repair is successful.
VITREORETINAL SURGERY
Vitreoretinal surgery encompasses a wide range of conditions that require treatment within the interior and back portion of the eye. These include:
- Vitreomacular Traction
- Macular Hole
- Epiretinal membrane
- Retinal Detachment
- Vitreous haemorrhage
- Complex Cataract Surgery/Secondary intraocular lens implants
“Vitrectomy” is one type of vitreoretinal surgery, and involves careful removal of the vitreous from the eye. At the end of a vitrectomy operation, the back of the eye may be filled with either clear fluid, gas, air or uncommonly silicone oil.
In cases where gas or air is used, vision may be hazy until the gas or air bubble dissolves by itself over one or two weeks.
- Due to concerns of increased eye pressure, patients are unable to fly, go up high altitudes, go scuba diving or receive nitrous oxide anaesthetic during this time.
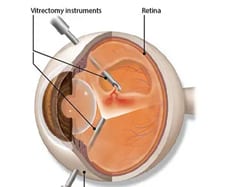
In the uncommon circumstance that silicone oil is required, vision will be blurred until it is removed through another procedure, often after a few months.
Patients may be advised to posture their head a certain way for the following days and/or nights after surgery. This is important to assist in the success of the surgery (e.g. after macular hole or retinal detachment repairs).
Retinal Detachment
Retinal detachment (as opposed to vitreous detachment described above) is a serious, vision-threatening condition where the retina detaches from the eye wall, causing loss of vision.
The vast majority of cases are due to retinal tears or holes allowing fluid to seep underneath the retina, causing the retina to progressively detach, a bit like ‘badly-applied’ wallpaper.
Symptoms may begin with flashes and/or floaters (see above), and/or a shadow may appear from the edges of the vision indicating a detached retina.
Patients may not have any of these symptoms and may only notice sudden vision loss, particularly in cases where it has rapidly progressed or has been left unnoticed.
Prompt surgery is required to repair the retinal detachment to restore their vision and eye.
Vitreomacular traction
The macula is the central portion of the retina, which is responsible for our clearer, detailed central vision.
Vitreomacular traction (VMT) is a condition where the vitreous only partly detaches, and there is abnormal vitreous adhesion, creating traction that pulls on the centre of the macula. This results in centrally blurred or distorted vision. Surgery may be indicated to relieve the traction, prevent worsening and allow the macula to resume a more normal shape.
Macular Hole
Macular hole is a condition where abnormal vitreous adhesion has created enough traction to pull a full-thickness hole in the central part of the macula. This results in severely blurred or distorted central vision. Macular hole is serious condition that is treated with day-surgery to relieve traction around the hole, and help close the hole with a gas bubble placed in the eye. The gas reabsorbs and is replaced by liquid, restoring vision.
If surgery is delayed or left untreated, an open macular hole may result in poor vision long-term.
Epiretinal Membrane
Epiretinal membrane is a common condition whereby a thin ‘cellophane-like’ membrane, may appear on the surface of the macula. This membrane can contract, distorting the normal shape of the macula. It often slowly progresses to cause blurred or distorted central vision. Many cases can be safely monitored, but if patients have significant symptoms, surgical peeling of the epiretinal membrane may be indicated to prevent worsening, and in some cases result in improvement of their symptoms. Your eye doctor will be able to advise the best course of action for you.
Vitreous haemorrhage
This is a bleed within the vitreous gel that may occur due to various reasons, including retinal tears, diabetic retinopathy, retinal vein occlusions, injury, and age-related macular degeneration.
This often results in dark, cloudy and/or blurred vision. Some cases can be carefully monitored, but surgery is often indicated to clear the vitreous haemorrhage, carefully examine for the underlying cause and to provide treatment if possible.
Complex Cataract Surgery/Secondary Intraocular Lenses
Routine cataract surgery involves placing an intraocular lens within the eyes normal structural support of the lens called the capsular bag. In some (‘complex’) circumstances, including trauma or other eye conditions, the capsular bag may be compromised or damaged, making it inappropriate to place the lens in the usual position. In these cases, implantation of secondary intraocular lenses may be required.
Secondary lens implantation involves surgically performing vitrectomy (see earlier) and securing an intraocular lens in a different location, either in front of the iris, on the iris, or behind the iris fixated to the sclera (outer wall of the eye).
